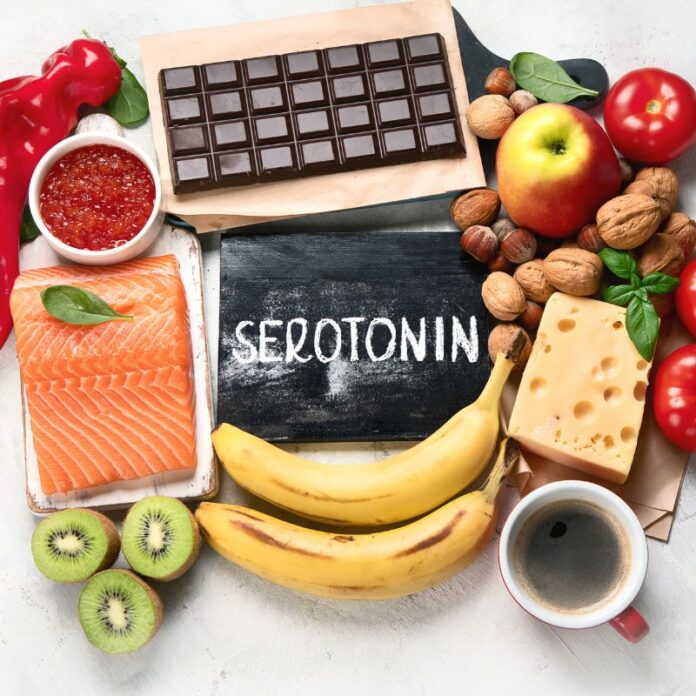
Migraines are more than just headaches—they’re a complex neurological condition that can debilitate daily life. While medications and lifestyle modifications are mainstays of migraine management, emerging research shows that nutrition—particularly the dietary factors that influence serotonin, a key neurotransmitter—can play a powerful role in reducing migraine frequency and severity.
In this comprehensive guide, you’ll learn:
-
How serotonin relates to migraine pathophysiology
-
Which nutrients and foods support healthy serotonin levels
-
Dietary patterns shown to benefit migraineurs
-
Practical meal and snack ideas to stabilize serotonin
-
Precautions, triggers to avoid, and tips for success
Let’s dive in.
Understanding Migraine and Serotonin
Serotonin (5-hydroxytryptamine, 5-HT) is a brain chemical that regulates mood, sleep, pain perception, and vascular tone. In migraines, serotonin’s role is twofold:
-
Baseline Serotonin Depletion: Many migraine sufferers have chronically lower interictal (between attacks) serotonin levels, which predispose them to attacks.
-
Ictal Serotonin Surge: During an attack, serotonin spikes temporarily, causing complex vascular changes—initial vasoconstriction followed by vasodilation—that precipitate pain.
Because diet provides the raw materials for serotonin synthesis, optimizing intake of key precursors (e.g., tryptophan), cofactors (e.g., vitamins B6, C), and supportive nutrients (e.g., omega-3s, magnesium) may help maintain more stable serotonin levels and reduce migraine risk.
Key Nutrients for Serotonin Production
1. Tryptophan: The Direct Precursor
-
Role: Tryptophan is an essential amino acid converted into 5-HTP and then serotonin in the brain.
-
Sources: Poultry, eggs, dairy, nuts, seeds, soy, and oats.
-
Evidence: A large case-control study (n=514) found that migraineurs consumed less dietary tryptophan than controls, suggesting adequacy may influence attack frequency.
Tip: Combine tryptophan-rich foods with complex carbohydrates to boost its uptake into the brain (insulin drives competing amino acids into muscle).
2. Vitamin B6 (Pyridoxine)
-
Role: A cofactor in the conversion of 5-HTP to serotonin.
-
Sources: Chickpeas, tuna, bananas, fortified cereals, and beef.
-
Clinical Insight: Low B6 has been correlated with poor neurotransmitter balance; supplementation (50–100 mg/day) may support mood and migraine control.
3. Vitamin C
-
Role: Required for the enzyme that synthesizes serotonin; potent antioxidant that protects neurotransmitter-producing cells.
-
Sources: Citrus fruits, bell peppers, strawberries, broccoli.
-
Supporting Data: Vitamin C deficiency impairs 5-HT synthesis; adequate intake correlates with better neurological function.
4. Omega-3 Fatty Acids
-
Role: Integrate into neural membranes, influencing serotonin receptor function and reducing neuroinflammation.
-
Sources: Fatty fish (salmon, mackerel), flaxseeds, chia seeds, walnuts.
-
Clinical Evidence: A 182-person RCT found that increasing omega-3s and reducing omega-6s led to up to 40% fewer migraine days over 16 weeks—comparable to fish oil supplements.
5. Magnesium
-
Role: Modulates NMDA receptors and serotonin release; deficiency linked to cortical spreading depression (migraine trigger).
-
Sources: Leafy greens, nuts, seeds, legumes, whole grains.
-
Research: Trials of 400–600 mg/day magnesium reduced migraine frequency by ~40% in up to 50% of participants.
Foods and Dietary Patterns That Support Serotonin and Reduce Migraines
Mediterranean-Style Eating
A wealth of evidence associates the Mediterranean diet—high in fruits, vegetables, whole grains, legumes, nuts, olive oil, and fish—with lower migraine prevalence. Its strengths include:
-
Rich Tryptophan & Cofactors: Legumes and fish
-
Antioxidant Power: Colorful produce combats oxidative stress in neurons
-
Healthy Fats: Olive oil and omega-3s reduce neuroinflammation
Low-Glycemic Meals
Rapid blood sugar swings can trigger migraines via stress hormone release. Choosing low-GI carbohydrates (e.g., steel-cut oats, quinoa, lentils) with protein keeps insulin and serotonin precursors on track .
Regular, Balanced Intake
Skipping meals is a well-known migraine trigger. Eating every 3–4 hours with balanced macros (protein, fiber, and healthy fats) maintains steady blood sugar and consistent serotonin synthesis .
Elimination and Personalized Triggers
Certain foods (tyramine-rich cheeses, processed meats, MSG, aspartame) may exacerbate migraines by affecting serotonin receptors or vasoactive peptides. An elimination diet can help identify personal triggers, as small studies have shown improved outcomes in select individuals .
Practical Meal and Snack Ideas
Breakfast: Serotonin-Stabilizing Smoothie
-
1 cup Greek yogurt (protein, tryptophan)
-
1 banana (B6)
-
1 Tbsp ground flaxseed (omega-3)
-
Handful spinach (magnesium)
-
Dash of cinnamon (stabilizes blood sugar)
-
Blend with water or fortified plant milk
Snack: Tryptophan-Rich Energy Bites
-
Rolled oats, almond butter, ground chia seeds, honey, and dried cherries
-
Roll into balls and refrigerate
Lunch: Mediterranean Chickpea Salad
-
Chickpeas (protein, tryptophan)
-
Cherry tomatoes, bell peppers (vitamin C)
-
Cucumber, red onion
-
Olives, feta, olive oil–lemon dressing (healthy fats)
Afternoon Snack: Nutty Banana–Date Plate
-
Sliced banana with a handful of almonds and dates (extra B6 and magnesium)
Dinner: Salmon and Veggie Grain Bowl
-
Baked salmon (omega-3, tryptophan)
-
Quinoa or brown rice (complex carbs)
-
Roasted Brussels sprouts and broccoli (vitamin C, fiber)
-
Drizzle of extra-virgin olive oil
Evening Treat: Chamomile-Serotonin Tea
-
Chamomile tea with a squeeze of lemon and a touch of honey can support relaxation and provide a gentle carbohydrate boost to steady insulin.
Lifestyle Factors that Complement Diet
-
Sunlight and Exercise:
Sun exposure aids vitamin D synthesis (cofactor for serotonin), and moderate exercise boosts tryptophan availability in the brain. -
Stress Reduction:
Mindfulness meditation and yoga lower cortisol, which can otherwise deplete serotonin stores. -
Adequate Sleep:
Serotonin is the precursor to melatonin; poor sleep disrupts this cycle and may increase migraine risk.
Potential Risks and When to Consult a Professional
-
Supplements Overuse: High‐dose 5-HTP or serotonin precursors can cause serotonin syndrome—always consult your doctor.
-
Drug Interactions: If you take SSRIs, triptans, or MAO inhibitors, dietary changes may alter drug effects—seek medical guidance.
-
Underlying Conditions: Unexplained migraines warrant evaluation to rule out secondary causes.
Conclusion
While migraines arise from multifactorial origins, nutrition—particularly the role of serotonin—offers a non-pharmaceutical avenue to reduce attack frequency and severity. By focusing on tryptophan-rich foods, essential cofactors (B6, C), anti-inflammatory omega-3s, and stabilizing blood sugar with balanced meals, you can support serotonin homeostasis and empower your brain’s resilience against migraines.
Combining these dietary strategies with hydration, stress management, regular exercise, and good sleep hygiene creates a holistic, sustainable approach to migraine relief. As always, personalize your plan—monitor patterns, identify triggers, and consult a healthcare professional to optimize your path to fewer, milder migraines. Here’s to eating your way to better days—one serotonin-boosting bite at a time.
Disclaimer
This article is intended for informational purposes only and does not replace professional medical advice. Always consult a healthcare provider before making significant changes to your diet or supplement regimen, especially if you have chronic migraine or are on medication.